The Real Story Behind Resident Doctors' Pay Before the 5-Day NHS Strike
The NHS Doctors' Pay Dispute: A Clash of Statistics and Priorities
The ongoing dispute between the British Medical Association (BMA) and the UK government over resident doctors’ pay has sparked significant controversy, with both sides using different statistical measures to justify their positions. As a result, the debate has become increasingly complex, raising questions about the accuracy of the data being used and the potential impact on the National Health Service (NHS).
Resident doctors, who are also known as junior doctors, have announced a five-day strike starting this Friday, demanding salary increases that could reach up to £20,000. They argue that these hikes are necessary due to what they describe as "pay erosion" over the past 17 years. According to the BMA, this erosion amounts to more than a 29% reduction in real terms. However, the government claims that resident doctors have already received an average pay rise of 28.9% over the last three years, including a 5.4% increase this year—making it the largest in the public sector.
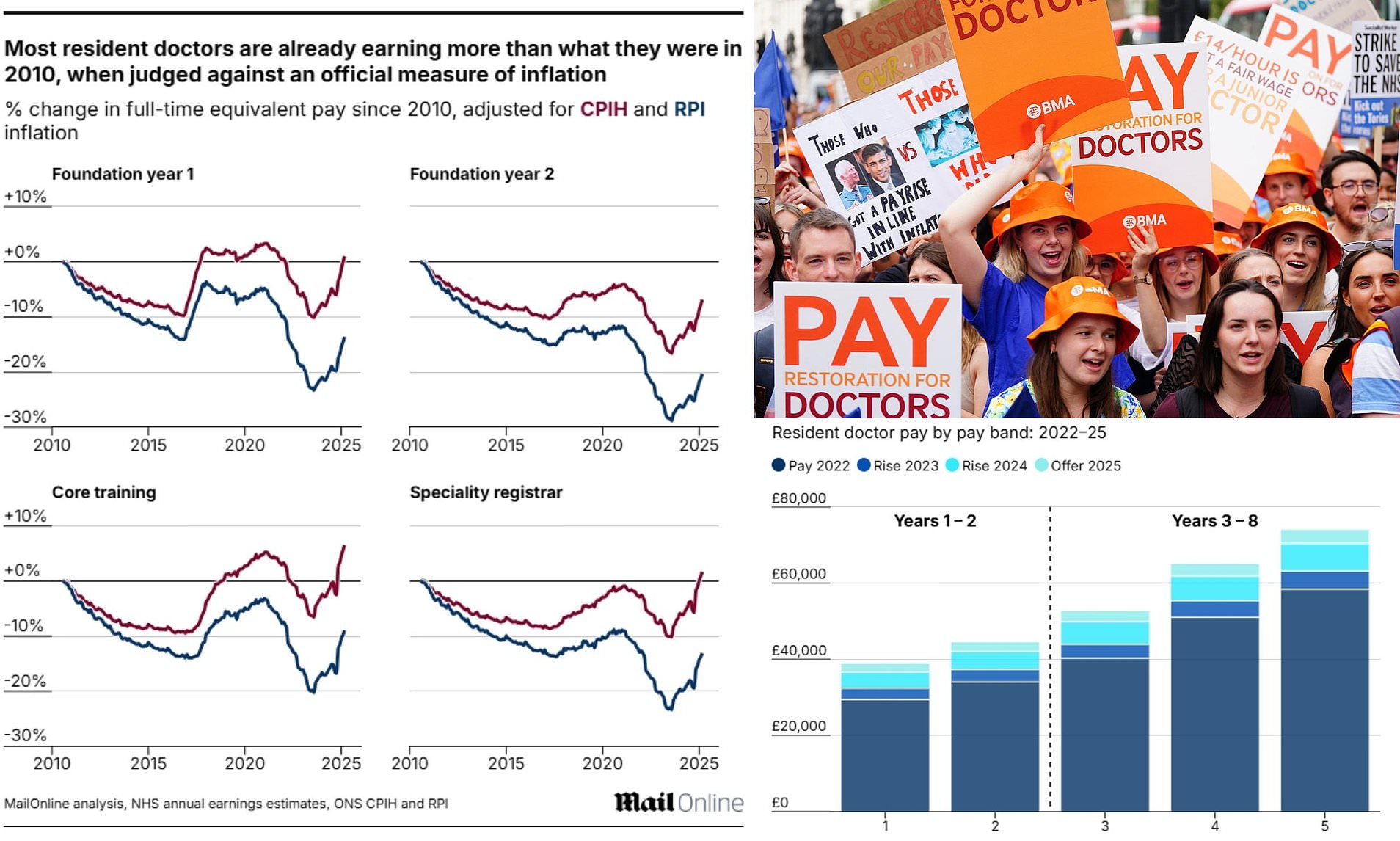
The BMA’s stance is that the current pay levels do not reflect the true cost of living for doctors, particularly given the high student loan debt many face upon entering the profession. The union uses the Retail Price Index (RPI) to calculate this erosion, which they argue better reflects the everyday expenses of working people. However, the Nuffield Trust, an independent health policy think tank, found that when measured against the Consumer Price Index (CPI), the pay gap is much smaller—only 4.7% below inflation since 2008. This discrepancy highlights the importance of the inflation measure used in such calculations.
The government has criticized the use of RPI, pointing out that it was downgraded as an official national measure in 2013 due to its tendency to overstate inflation. Instead, CPI and CPIH (which includes housing costs) are now considered more accurate. Despite this, the BMA continues to defend its use of RPI, arguing that it is more relevant to the daily lives of doctors. For instance, RPI is used to set student loan repayments, car taxes, and train fare caps—factors that significantly affect the financial burden of medical professionals.
Health Secretary Wes Streeting has condemned the strikes as "shockingly irresponsible," insisting that the government will not compromise on pay. He emphasized that resources are finite and that decisions must be made with the interests of all NHS staff in mind. Streeting also pointed out that resident doctors have already received substantial pay increases under the current administration, including a 28.9% rise over three years.
Despite these efforts, the BMA remains unconvinced. In September, members voted overwhelmingly in favor of further strike action after rejecting a proposed pay deal from the government. The latest offer included a 4% uplift plus £750 in additional payments, resulting in an average pay increase of 5.4%. However, this was not enough to prevent another round of industrial action, with nearly 90% of those who voted supporting the walkout.
The consequences of the strikes are expected to be severe. A report by the Policy Exchange think-tank warned that up to 250,000 appointments could be canceled or postponed this month, costing the NHS approximately £87 million in staffing cover. Charities have also expressed concern, warning that the disruptions could lead to "significant distress, pain, and worsening health for patients."
In addition to the financial impact, there are serious safety concerns. Previous strikes by junior doctors have been linked to at least five patient deaths, according to an audit. NHS leaders have warned that the upcoming five-day walkout could put even more lives at risk.
As the debate continues, the question of how to fairly assess pay increases remains unresolved. Different inflation measures can paint vastly different pictures of real-term changes in wages, making it essential to consider multiple perspectives. The Nuffield Trust's Lucina Rolewicz emphasized the need to look at a range of baseline years and inflation measures to gain a more complete understanding of the situation.
Ultimately, the dispute underscores the challenges of balancing the needs of medical professionals with the broader responsibilities of the NHS. While the BMA argues that fair pay is crucial for retaining talent and ensuring quality care, the government maintains that resources must be allocated wisely across the entire healthcare system. The outcome of this conflict will likely have far-reaching implications for both the NHS and the wider public.