About the Experts
Astrid Werner, MD, is an ophthalmologist and the Vice Chair of Clinical Services at New England Eye Center at Tufts Medical Center and assistant professor of ophthalmology at Tufts University School of Medicine. Meredith R. Klifto, MD, is an assistant professor of ophthalmology at the University of North Carolina School of Medicine, Chapel Hill. As a board-certified ophthalmologist, she specializes in treating cataracts, glaucoma, and ocular trauma. Yuna Rapoport, MD, MPH, is a board-certified ophthalmologist and the founder of Manhattan Eye. She’s also an assistant clinical professor of Ophthalmology at Mount Sinai in New York City and has been named one of the best Lasik surgeons in America. Andrew Iwach, MD, is a clinical spokesperson for the American Academy of Ophthalmology (AAO). He’s also an associate clinical professor of ophthalmology at the University of California at San Francisco, a faculty instructor at the California Pacific Medical Center Department of Ophthalmology, and the Executive Director of the Glaucoma Center of San Francisco. Noah Rosen, MD, is a board-certified neurologist and psychiatrist with additional boards in headache and pain medicine. He is the vice chair of neurology at Northwell Health and the director of Northwell Health’s Headache Center in Great Neck, New York. He is also an associate professor at the Zucker School of Medicine at Hofstra University.
Highlights
When it comes to eye problems, blurry vision is the most common visual symptom. There are many potential causes of blurry vision—some are harmless, but others can indicate a serious issue. Blurry vision is often treatable, and in some cases, doctors can fix the issue entirely. No matter the cause of blurry vision, outcomes are best when it’s identified and treated as soon as possible.
Blurry vision is a general term people use to describe a loss of visual sharpness, explains Astrid Werner, MD, ophthalmologist and Vice Chair of Clinical Services at New England Eye Center at Tufts Medical Center. “People often start out by saying things like: ‘It’s like looking through a foggy window,’ or ‘It’s like I have a film over my eyes,’ or ‘Things just aren’t crisp anymore.’” But depending on the cause, that description can vary, she says—especially if you probe a bit further. “The details matter when it comes to understanding the patient’s exact experience of blurry vision.”
And, Dr. Werner says, dialing into the exact cause of blurry vision is important. It’s the most common visual symptom there is, with a range of possible causes—many of which are correctable or even fixable. “But unfortunately, there are also many causes of blurry vision where the damage is irreversible,” she explains. “We do have treatments to halt or slow down the progression of these [causes], so that’s why routine eye exams are so important to catch problems early.”

1. Refractive Errors
The most common cause of blurry vision is a refractive error, Dr. Werner says. There are four main types of refractive errors, according to the National Eye Institute (NEI):
- Nearsightedness or myopia: objects in the distance are blurry
- Farsightedness or hyperopia: objects nearby are blurry
- Astigmatism: images look blurry or distorted
- Presbyopia: a condition that makes it hard for people to see things up close as they age
The NEI says that more than 150 million Americans have a refractive error, but many more don’t realize they could be seeing better. That’s why regular eye exams are important. Untreated refractive errors, even if they’re mild, can contribute to uncomfortable eye strain and headaches.
“This is the first thing to rule out [if you have blurry vision] and the most easily corrected,” explains Meredith R. Klifto, MD, assistant professor of ophthalmology at the University of North Carolina School of Medicine, Chapel Hill. This type of blurry vision is often easily fixed with glasses or contacts, Dr. Werner says. “Refractive error can also be corrected with simple refractive procedures such as LASIK, SMILE, RLE, and ICL,” adds Yuna Rapoport, MD, MPH, founder of Manhattan Eye and an assistant clinical professor of ophthalmology at Mount Sinai in New York City.

2. Cataracts
Almost everyone will get cataracts if they live long enough, says Andrew Iwach, MD, a clinical spokesperson for the American Academy of Ophthalmology (AAO). Over time, the lens of your eye gets cloudy, making it harder to see. Blurred vision may be one symptom. “Someone with cataracts might mention cloudiness or glare, starbursts, or halos around lights, often noting that these symptoms are worse at night—and that driving at night is particularly difficult,” Dr. Werner says. Cataracts can also make it hard to read in dim light, Dr. Klifto adds.
Fortunately, cataracts are curable. “It’s about a 20-minute outpatient procedure,” says Dr. Klifto. “They put in a new artificial lens that’s the perfect power for you based on measurements we take pre-operatively.” In other words, the procedure not only gets rid of the cataract, it often corrects your vision as well.
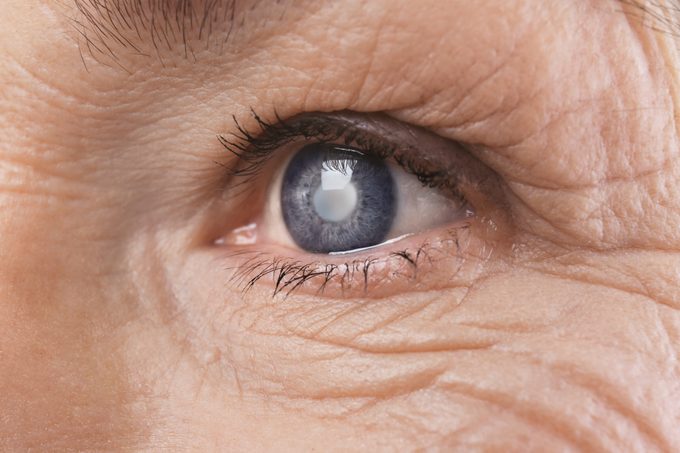
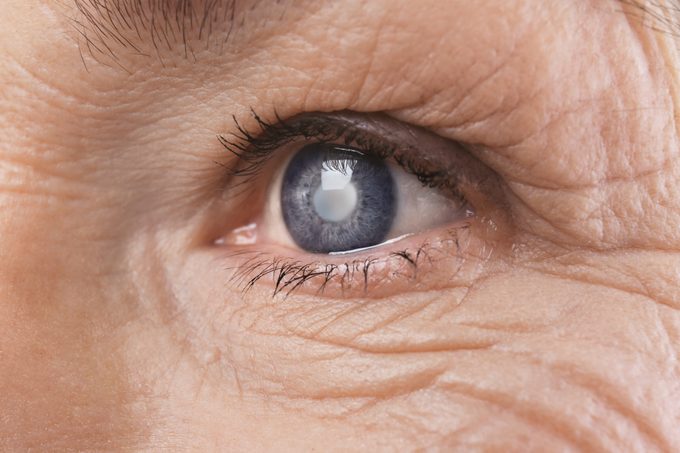
3. Glaucoma
Glaucoma is a group of eye diseases that damage the optic nerve, often, but not always, due to elevated eye pressure, Dr. Werner explains. “Early on, patients don’t notice anything—but over time, it slowly steals peripheral vision,” she says. By the time glaucoma affects central vision and causes noticeable blurring, the damage is often advanced and irreversible. “That’s why we sometimes call it the ‘silent thief of sight.’”
In addition to vision loss, the Cleveland Clinic says that glaucoma can cause other symptoms, such as:
- Eye pain or pressure
- Headaches
- Red or bloodshot eyes
However, these symptoms also don’t usually occur until there’s irreversible damage to the eye. There are certain factors, such as family history and advancing age, that can increase the risk of developing glaucoma. Glaucoma isn’t curable, but treatments can help slow or even stop its progression, Dr. Werner says. These treatments include medications, laser procedures, and surgical options.

4. Age-related Macular Degeneration
“Macular degeneration causes deterioration of the central part of the retina—the macula—which is responsible for sharp, detailed vision,” Dr. Werner explains. “It’s a degenerative condition that worsens over time.” And, as the name suggests, it becomes more common with age. She says that people with this condition might say that faces look blurry or that words on a page are hard to read. “Some even notice a dark or blank spot in the center of their vision.”
Dr. Werner says that macular degeneration comes in two forms:
- Dry macular degeneration: The cells in the central retina become damaged and atrophy over time.
- Wet macular degeneration: Abnormal blood vessels form under the retina and can leak into the layers of the retina.
“The dry form often causes a more gradual loss of clarity over time, while the wet form can cause rapid changes in vision, such as distortion (straight lines looking wavy) or dark spots in vision,” she says. “There are treatments for both forms of macular degeneration, so again, early detection and treatment are critical.”
Age, a family history of the eye disease, and having light-colored irises are risk factors for macular degeneration. However, the American Macular Degeneration Foundation (AMDF) says that other risk factors are controllable, including:
- Smoking
- Being overweight
- High blood pressure
- Sun exposure without protective eyewear

5. Eye Strain
Computers, smartphones, and tablets—these days, screens, in general, are a common cause of dry eye, which, in turn, is a common cause of blurry vision. “When we blink, our usual blink rate is 18 times per minute,” Dr. Rapoport says. “When we are on a screen, our blink rate decreases to eight times per minute, which can cause our corneas to dry out.” She explains that excessive dryness can cause irregularities in the cornea’s normal smooth surface—and when that happens, light scatters in different directions, contributing to blurry vision. “Dry eye is a chronic inflammatory condition, and in the long run can cause permanent damage.” Taking screen breaks every 20 minutes to give your eyes a chance to blink, says Dr. Klifto. Eye drops can also help—but stay away from products that say “get the red out,” she adds. They can actually make the problem worse. You likely specifically need a drop for dry eye, which a doctor can recommend.

6. Home Improvement Projects
“More eye injuries have now shifted to the home,” says Dr. Iwach. That’s because people are doing DIY projects at home, often finding experts’ instructions online, but these folks are often not wearing protective eye gear. “With high-velocity tools, small fragments can get embedded in the tissue,” he explains. Children are particularly at risk—they’re just at the right height, and they’re curious. Of course, any kind of eye trauma can cause blurry vision. Sports or recreational activities cause more than 40% of eye injuries, and overall, 78% of victims weren’t wearing any eyewear, including protective gear, when they were injured, according to the AAO. So, wear protective eye gear, and keep in mind that blurry vision could be the least of your problems if you do experience eye trauma.

7. Allergies
Itchy, runny eyes are a classic symptom of allergies, but allergies can also cause blurry vision. “Common environmental allergens that can cause eye allergies are pollen, mold, dust mites, and pet dander,” Dr. Werner says. “There are also bacteria and mites called Demodex that can live on the eyelids and lashes that can cause irritation and allergy-like symptoms.” “[Because of] irritation, oftentimes people rub their eyes, and that can impact vision,” says Dr. Iwach. But inflammation also plays a role. “Inflammation from allergies or other irritants cause blurry vision by disrupting the delicate balance of the tear film, making the ocular surface no longer smooth,” Dr. Werner explains. “This can lead to fluctuating, hazy vision, especially when blinking or rubbing the eyes.” Fortunately, eye allergies are temporary, and you can get relief with over-the-counter antihistamines and eye drops. The eye drops should be artificial tears (again, not the “get the red out” versions) and preservative-free, stresses Dr. Klifto.

8. Contact Lenses
“Contact lens wearers are at increased risk of sight-threatening infections,” Dr. Werner says. In serious cases, these infections can even cause a corneal ulcer, which, if left untreated, can cause vision loss and blindness, per the Cleveland Clinic. “Wearing contacts while sleeping, showering, or swimming greatly increases the risk of vision-threatening infections, and you should never clean your contacts with tap water or saliva,” Dr. Werner emphasizes. Social media has revealed how microorganisms in water can “Any vision changes accompanied by pain, irritation, or redness should be a sign to discontinue use of your contacts and seek care immediately.” If you’re taking care of your contact lenses and using them as instructed, you shouldn’t have problems. According to the AAO, this care includes:
- Always cleaning and disinfecting your contact lenses before putting them in your eye with a sterile lens cleaning solution
- Throwing them out when they expire
- Not sleeping in daily wear lenses
- Changing your case at least every three months (or right away if it gets cracked or damaged)
- Avoiding anything where water gets in your eyes while wearing contacts
And if you’re in the mood for decorative lenses for Halloween or another special occasion, make sure you get them from an ophthalmologist. Also, make sure you have a pair of backup glasses. That way, if your eyes get irritated, you can take a break, says Dr. Iwach.

9. Diabetic Retinopathy
Diabetic retinopathy can be a long-term complication of poorly controlled diabetes, and it can cause blurry vision. It’s the result of chronically high blood sugar levels, which erode the vessels in the retina, explains the National Eye Institute. Early diabetic retinopathy has no symptoms, and that’s why the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends that people with type 2 diabetes see an eye doctor annually. There are treatments but no cure for diabetic retinopathy. Your best bet is to try to prevent it by controlling your diabetes, although this isn’t always enough. “Even if diabetes is controlled, you can, over time, develop diabetic retinopathy,” says Dr. Iwach. “The better you control your diabetes, it helps delay or reduce the risk but, it’s not 100 percent.” Diabetes can also cause glaucoma and macular degeneration.

10. Herpes
Although infection with the herpes simplex virus (HSV) is more often associated with genital herpes and cold sores, it can also affect your eyes and cause blurry vision, along with pain, redness, lesions around your eyes, and sensitivity to light, says Dr. Klifto. Like herpes in other parts of your body, ocular herpes lies dormant for periods of time and then is activated, possibly because of stress or if your immune system has been weakened. Eye herpes is caused by HSV-1, which is the same virus that causes fever blisters. (HSV-II causes genital herpes, according to the Kellogg Eye Center at Michigan Medicine.) Once you have herpes, it never goes away, but outbreaks can be controlled with antiviral ointments or sometimes steroids, says Dr. Klifto.

11. Pink Eye (conjunctivitis)
Pink eye, or conjunctivitis, is an infection in the eye. Conjunctivitis can be caused by viruses, bacteria, or allergies—but viruses are most common, says the Mayo Clinic. It’s called “pink eye” because as your eyes become inflamed, they take on a red or pink hue. Also, says Dr. Klifto, “There’s a lot of tearing, redness, discharge, not just blurry vision.” Most cases of pink eye—both viral and bacterial—will go away on their own within ten days to two weeks, according to the Cleveland Clinic. But if your pink eye symptoms aren’t improving or are getting worse after a few days (like ongoing eye discharge, severe discomfort, or a fever), you should see your primary care provider. Depending on what’s causing your pink eye, your doctor may prescribe antibiotics, an antiviral, or an antifungal drug to speed up healing. As your pink eye heals, the Cleveland Clinic says that over-the-counter eye drops (or “artificial tears”) and warm or cool compresses can help manage discomfort. In addition, it’s important to keep the infection from spreading to others: Wash your hands often, don’t touch your eyes, don’t share towels, and don’t share makeup.

12. High Blood Sugar
“High blood sugar in extremes can cause blurry vision,” says Dr. Iwach. “Fortunately, it’s not as common as it used to be.” Dr. Rapoport explains that high blood sugar in the short run causes the lens inside our eye to swell, which leads to vision fluctuations. This blurriness should go away on its own when your blood sugar levels get back to a healthy range, according to the AAO. It’s another potential complication of diabetes, but usually a short-term one. However, chronically high blood sugar can cause serious retinal issues like bleeding and swelling, Dr. Rapoport says. “[This] then has to be treated with injections and lasers.” People with diabetes may temporarily get blurry vision for a few days or weeks if they’re changing their medication, notes the NIDDK. This underscores the importance of keeping type 2 diabetes in check with proper diet, exercise, and medication. If you have diabetes, the AAO also recommends getting regular eye exams to catch any potential problems early, when they’re most treatable.

13. High Blood Pressure
Similar to high blood glucose, high blood pressure in extremes can cause blurry vision. “You can have very high blood pressure, and that can affect the refractive status of the lens,” explains Dr. Klifto. Over time, high blood pressure damages the small vessels in the eye, restricting blood flow to the area and damaging the retina (the structure in the back of the eye that receives light), according to the Merck Manual. This is just one possible result of chronic hypertension. Others include heart attack, stroke, heart failure, kidney disease, problems with sexual function, and angina, says the American Heart Association.

14. Migraine
Blurry vision can be part of the aura state that sometimes comes right before or at the beginning of a migraine, says Noah Rosen, MD, director of Northwell Health’s Headache Center in Great Neck, New York. Other visual symptoms can include zig-zag lines and double vision. “These tend to be transient and only in a brief period,” he says. Usually, these ocular symptoms aren’t dangerous (unless you’re driving). “Timing is important,” says Dr. Rosen. “Most of the time [visual disturbances] improve in five minutes to an hour and an average of 20 minutes, but if it’s prolonged, it should probably be checked out.”

15. Medications
While rare, some medications can cause problems in your eye’s retina—and if you take them, you need to check in with your eye doctor yearly, Dr. Rapoport says. These include:
- Plaquenil, a drug used to prevent and treat malaria, as well as some autoimmune conditions like rheumatoid arthritis
- Thorazine, an anti-psychotic medication
- Niacin, a B-complex vitamin that is used to treat high cholesterol
- Tamoxifen, a breast cancer medication
- Canthaxanthin, a drug used to reduce sensitivity to sunlight
- Sildenafil, which is sold under the brand name Viagra
Dr. Rapoport says that many medications can also cause dry eye, including anti-hypertensives, hormonal medications (including oral contraceptives), and anti-depressants or anti-psychotics. Dry eye can feel like just a mild inconvenience, causing discomfort and blurry vision (especially in dry environments). But if left untreated, dry eye can lead to damage on the surface of your eye, increase the risk of eye infection, and potentially cause permanent vision issues. If you’re experiencing dry eye as a side effect of your medication, it’s important to talk with your doctor about how to manage and treat the condition. You may also be able to switch to a different medication with less risk of this side effect.

16. Scratched Cornea
A scratched cornea—or corneal abrasion—is a tiny injury to the surface of the eye. “When the top layer of the cornea (the epithelium) is scratched away, the cornea is very irregular, and that causes blurry vision,” Dr. Rapoport says. Per the Cleveland Clinic, other signs of a scratched cornea include watery eyes, sensitivity to light, swelling, and a feeling that there’s something in your eye. “The most common cause of a scratched cornea is an injury from a fingernail,” she explains. But some people have a genetic disorder that affects the cornea called ABMD—Anterior Basement Membrane Dystrophy. This means that the top layer of cells doesn’t stick well to the layer beneath. “In this instance, patients can wake up with scratched corneas randomly,” Dr. Rapoport explains. “There are preventative measures we can take to make sure the scratches do not happen often.” “Healthy corneas do heal on their own, but it is better to treat with drops and ointment at the doctor’s office,” Dr. Rapoport says. This is because if the scratch turns into an infection, it can cause more serious damage.

When to See a Doctor
If you’re experiencing any vision changes, it’s always important to see an eye doctor. “Blurry vision can be harmless—sometimes it’s just dry eyes or needing glasses,” Dr. Werner says. But don’t self-diagnose or write it off. Even mild causes of blurry vision can worsen if left untreated, potentially leading to more serious damage and vision loss. Still, there are some cases when urgent medical attention may be required. “If [blurry vision] comes on suddenly, affects just one eye, or is associated with other symptoms like pain or light flashes—that’s when we get concerned,” she says. “It can be a sign of something more serious, like a retinal issue or even a stroke.” In fact, you might be surprised what diseases eye doctors may find first.
In general, Dr. Werner says that you should seek medical attention:
- Immediately if blurry vision is sudden, in one eye, or accompanied by other symptoms like pain, light flashes, floaters, or headache
- Soon (within a few days) if vision changes are mild but gradually worsening or not improving with blinking or rest
- Routinely if it’s related to a known cause—like needing new glasses—or for monitoring a chronic condition like diabetes, even if you don’t have any vision changes
“The bottom line is that if you are worried, seek care,” she stresses. “Your eyes are too important to take chances with!”