Woman Diagnosed with Cancer Just Six Days After Falling Ill on Vacation
A Rare Survivor's Journey
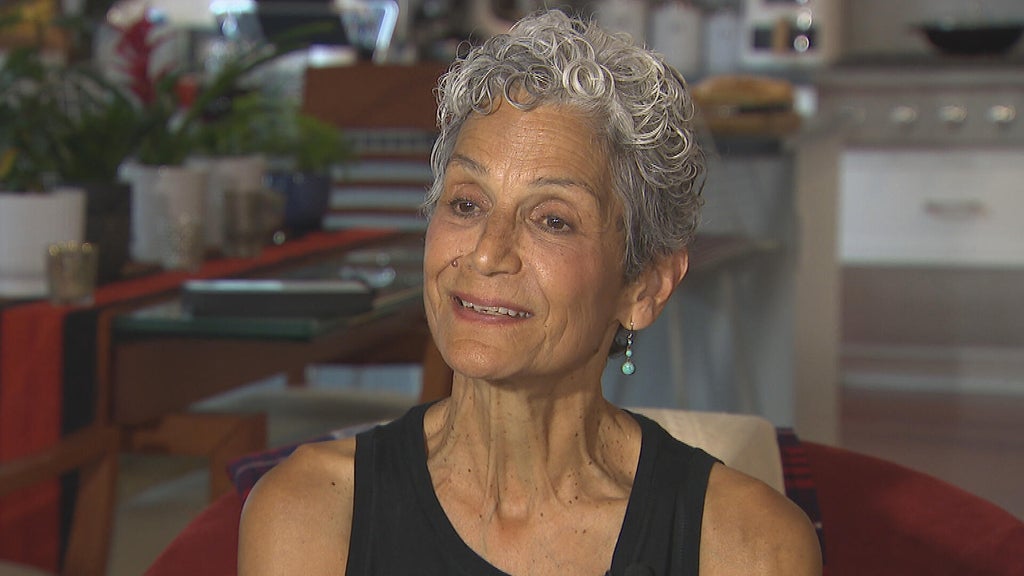
A retired nurse who was diagnosed with pancreatic cancer says she feels “incredibly lucky” to be a rare survivor of the disease, which has a five per cent survival rate long term. Suzanne Ford, 67, was on holiday in Nice, France, in September 2023, when she began feeling slightly unwell. She and her friends had been “eating, drinking, making merry, having a great time” on their trip, and though she’d felt generally well throughout, she began feeling a little queasy in the final days of the holiday, something she thought may be “over-indulgence”. However, when she came home to York, her symptoms began getting worse, and she noticed a change in the colour of her poo before developing a full-body itch.
“I am an ex-nurse, so that kind of alerted me that something might not be quite right, but I hadn’t a clue what was going on,” she said.

According to the NHS, pancreatic cancer may not have any symptoms, or they may be hard to spot. Symptoms can include jaundice, itchy skin, darker urine and poo than usual, loss of appetite, tiredness, diarrhoea or constipation, stomach pain and nausea. Suzanne went to her GP, who conducted some blood tests, and she returned to her nursing job. Just six days after experiencing her first symptom, she was booked in for a CT scan, which confirmed she had pancreatic cancer.
When Suzanne was diagnosed on October 3 2023, she was “devastated”. “I knew the futility of people who’ve been diagnosed late with pancreatic cancer in accessing treatment that could be life-saving,” she said. “So I knew that there could be a really poor outcome for myself.”

Indeed, according to Pancreatic Cancer UK, pancreatic cancer is the fifth biggest cancer killer in the UK. Despite it being the 10th most common cancer, it has the lowest survival of all common cancers, with five-year survival less than 7 per cent, as most people – 80 per cent – are diagnosed at stage three or four, when the cancer has spread. Doctors believed Suzanne’s cancer was stage two, and that it had had some localised spread within her pancreatic duct and her bile duct. Her gallbladder had become blocked by the tumour, so she had an intermediate stent put in to alleviate the effects of the blockage – at which point she felt “quite gloomy, because of the potential prospect of getting to treatment”.
“My husband and family did too,” she added. “They were all devastated. I had friends who had lost loved ones to pancreatic cancer, so I knew what I was dealing with, potentially.”

However, Suzanne was deemed to be in an operable state. According to Pancreatic Cancer UK, just one in 10 people with pancreatic cancer will receive potentially curative surgery – meaning Suzanne was very lucky to have been diagnosed early enough for treatment. On November 20 2023, she had “life-saving surgery” – an eight or nine-hour operation called a pancreaticoduodenectomy (PPPD), in which they effectively “replumb your insides”, removing part of the pancreas, the first part of the small bowel, the gallbladder and part of the bile duct before joining the tail of the pancreas to the small bowel. After the surgery, the pathology found that it was stage three, but with no local spread. Thankfully, Suzanne made a “very, very good recovery”. “Part of that might have been that I had been keeping myself fit and healthy before all this started, so that stood me in good stead, but I was looked after very well, and I was incredibly lucky that I didn’t develop any complications,” she said.

Within nine days, Suzanne was out of hospital, and had around two months’ recovery from her surgery before beginning chemotherapy for another eight months. “In my circumstance, the fact that my gallbladder was blocked and I was scanned so early on, although I had relatively mild symptoms, it saved my life,” Suzanne reflected. “If it had been left, it would have become inoperable, and I would have been another one of the statistics.” Suzanne felt “incredibly lucky” that her GP acted quickly in getting her the tests and scans she needed and contacting the necessary specialists to get her a diagnosis at the earliest possible stage, and she knows all too well how rare her circumstances are.
Her experience has made her particularly passionate about supporting the work of Professor George Hanna and his team at Imperial College who, with a £1.1 million investment from Pancreatic Cancer UK, are developing a world-first breath test for the disease that could be used in GP surgeries. Now, the test is at a stage where the team are able to conduct a large UK-wide clinical trial, and it is hoped that if successful, it could improve the prognosis of those diagnosed with pancreatic cancer.
Main Symptoms of Pancreatic Cancer
Symptoms of pancreatic cancer can include:
- the whites of your eyes or your skin turn yellow (jaundice), and you may also have itchy skin, darker pee and paler poo than usual
- loss of appetite or losing weight without trying to
- feeling tired or having no energy
- a high temperature, or feeling hot or shivery
- Other symptoms can affect your digestion, such as:
- feeling or being sick
- diarrhoea or constipation, or other changes in your poo
- pain at the top part of your tummy and your back, which may feel worse when you're eating or lying down and better when you lean forward
- symptoms of indigestion, such as feeling bloated
Suzanne said: “I think this is going to be a fantastic tool for GPs, because all these people who go with these vague symptoms again and again… For those patients who are at a suspected cancer risk, they will be able to do a breath test. The belief is that they’ll have results within three days, and then there’ll be a quick referral through for a CT scan, which will be definitive in seeing whether somebody looks like they’ve got pancreatic cancer or not. The difference that will make is it means that the percentage of people that are picked up early will rise, and those who (are diagnosed) will have a much better survival rate because they can get to treatment much earlier, hopefully.”
Anna Jewell, director of support, research & influencing at Pancreatic Cancer UK, said: “Suzanne’s story is proof that it is possible to live well after pancreatic cancer and enjoy all the wonderful things life has to offer, like precious time with her grandchildren. Tragically, too few people are currently diagnosed early enough for life-saving treatment because detecting the disease in its earliest stages is a huge challenge for doctors. Thousands of people with unknown symptoms are now helping to validate the breath test, and it will be several years before we know the outcome. But if the scientists are successful, and the test is then adopted by the NHS, the impact on early detection could be revolutionary. It could pave the way to thousands more people a year surviving the deadliest common cancer. The development of promising new tools like the breath test, and others, offers real, tangible hope for the future. To make that future possible we need to see a commitment from government for greater, consistent research investment included in the upcoming national cancer plan.”