Latest Listeria Outbreak Linked to Pregnancy Loss—What Expectant Moms Must Know
Understanding the Listeria Outbreak and Its Impact on Pregnant Individuals
A recent Listeria outbreak has raised concerns across the United States. As of late October, the Centers for Disease Control and Prevention (CDC) reported seven new illnesses and two additional deaths linked to this outbreak. The source of the contamination is prepared pasta products sold at grocery stores nationwide. To date, 27 people in 18 states have been infected, with 25 hospitalizations and six fatalities. Tragically, one individual who contracted Listeria lost her pregnancy.
For pregnant individuals, this situation can be especially alarming. However, there are steps that can be taken to minimize the risk of infection and protect both the mother and the unborn child. Below is a detailed breakdown of what you need to know about this outbreak and how to stay safe.
What to Know About the Food Contaminated by Listeria
According to the latest CDC update, 27 people have been infected during this outbreak. Of those interviewed, 54% reported eating precooked meals, and 57% said they had consumed chicken fettuccine alfredo. Many of these meals were purchased from Walmart or Kroger’s refrigerated section. Some also mentioned consuming salads containing pasta from various stores.
Dr. Zachary Hoy, a board-certified pediatric infectious disease specialist, advises everyone to check their refrigerators for any of the recalled items and discard them if found. He notes that some products may have “best by” dates as late as October 29. A full list of affected products is available on the FDA website.
Dr. Sharon Nachman, chief of pediatric infectious diseases at Stony Brook Children's Hospital, explains that Listeria is a type of bacteria that can contaminate food. “Typically, we see Listeria outbreaks associated with unwashed produce, raw milk, cheeses, and deli meats,” she says. “Infected foods do not always smell bad, but if food does smell bad, it should be thrown out.”
All the Foods Affected by the Recall
The FDA has issued recalls for several products associated with the outbreak. These include:
- Sprouts Farmers Market Smoked Mozzarella Pasta Salad: Use by dates from 10/10/25 through 10/29/25
- Giant Eagle smoked mozzarella pasta salad: Expiration dates from 9/30/25 through 10/7/25
- Scott & Jon’s Shrimp Scampi with Linguini Bowls (9.6 oz): Best if used by dates from 3/12/2027 to 3/21/2027
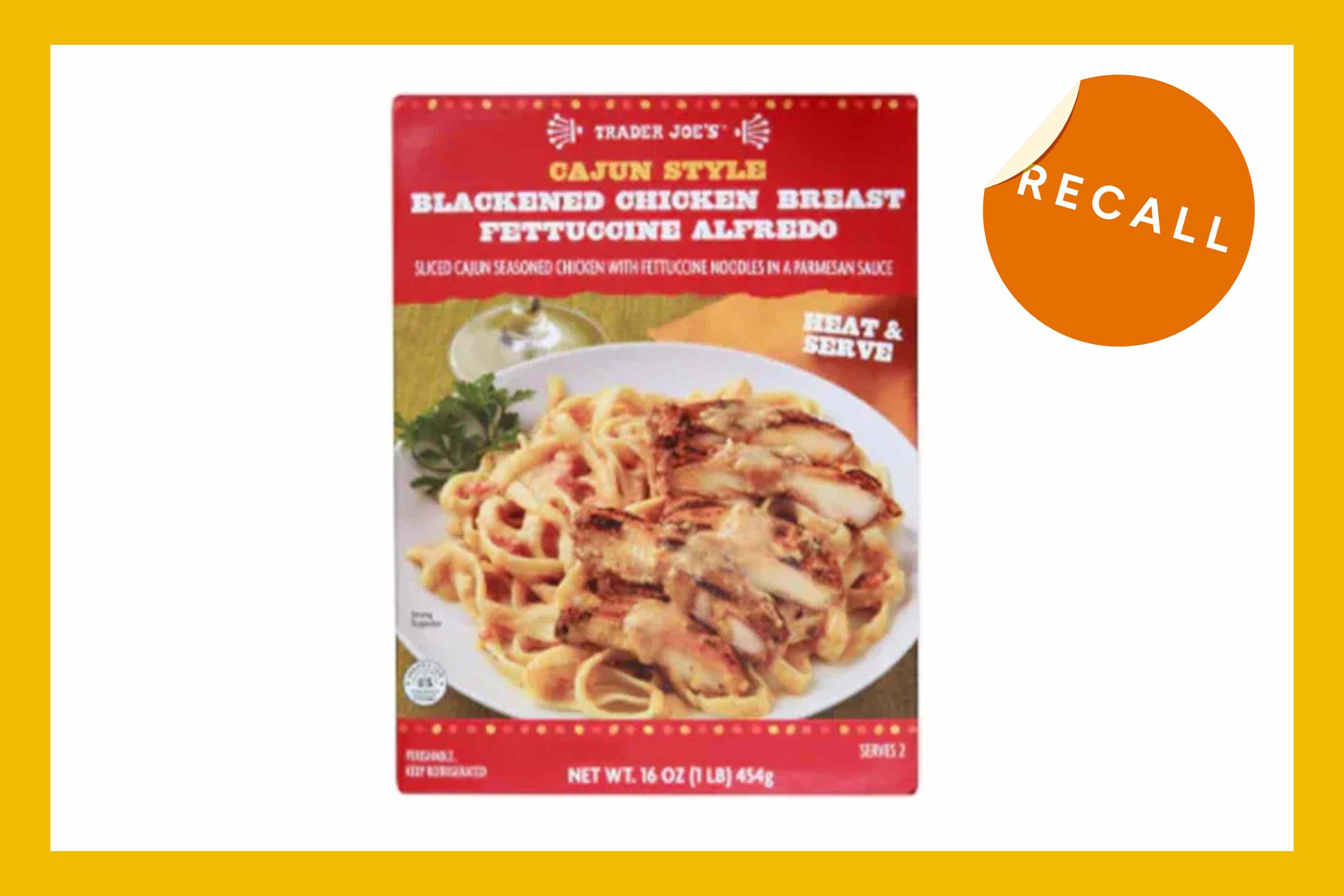
- Trader Joe’s Cajun Style Blackened Chicken Breast Fettucine Alfredo (16 oz): Best if used by dates from 9/20/2025 to 10/10/2025
- Marketside Linguine with Beef Meatballs & Marinara Sauce (12 oz): Best if used by dates from 9/22/25 to 10/1/25
- Marketside Grilled Chicken Alfredo with Fettuccine (12.3 oz and 32.8 oz): Best by dates up to 6/27/2025
- Home Chef Chicken Fettuccine Alfredo (12.5 oz): Best by date of 6/19/25 or prior
- Kroger deli bowtie and penne pasta salads: Recalled from August 29 through October 2, 2025
- Albertsons store-made deli pasta salads: Recalled with sell-by dates from September 8 to October 4, 2025
These products were sold at major retailers such as Walmart, Kroger, Albertsons, and Trader Joe’s.
What Else We Know About the Outbreak So Far
The outbreak began in June and was linked to prepared pasta dinners from food supplier Nate's Fine Foods. Cases have been reported in California, Florida, Hawaii, Illinois, Indiana, Louisiana, Michigan, Minnesota, Missouri, North Carolina, Nevada, Ohio, Oregon, South Carolina, Texas, Utah, Virginia, and Washington.
What Are the Risks of Listeria, and Who Is Most at Risk?
While most low-risk individuals infected with Listeria may not require medical attention, higher-risk groups face more severe complications. Dr. Shira Doron, chief infection control officer for Tufts Medicine, explains that symptoms for lower-risk individuals typically include intestinal issues like diarrhea, nausea, and vomiting. However, for high-risk individuals—such as pregnant women, newborns, people over 65, and those with weakened immune systems—symptoms can be more serious, including sepsis and meningitis.
What Are the Risks of Listeria to Pregnant People?
Pregnant individuals are at a significantly higher risk of contracting Listeria due to decreased immunity during pregnancy, according to Dr. Kecia Gaither, a double board-certified OB/GYN and maternal fetal medicine specialist. This increased vulnerability can lead to serious complications, including miscarriage, preterm delivery, severe newborn infections, stillbirth, or neonatal demise.
Symptoms of Listeria in pregnant individuals may resemble mild flu-like symptoms, such as headache, muscle aches, fever, nausea, vomiting, and diarrhea. Neurological symptoms, like stiff neck, disorientation, or convulsions, may also occur. Symptoms can appear days or even up to two months after exposure to contaminated food.
If you suspect exposure to Listeria, it is essential to consult your healthcare provider immediately. A blood test can confirm the infection, and early antibiotic treatment can reduce risks to the fetus.
Listeria Symptoms in Newborns
Newborns can contract Listeria from their mothers during delivery. If your baby shows any of the following symptoms, contact their pediatrician right away:
- Extreme fatigue
- Vomiting
- No appetite
- Yellowish skin or eyes
- A skin rash
- Any trouble breathing
Listeria in newborns is diagnosed through blood, urine, or cerebrospinal fluid testing. Antibiotics are used for treatment. While the risk of transmission through breastmilk is low, seek guidance from your pediatrician if you are infected and breastfeeding.
How Can Pregnant People Protect Themselves from Listeria?
Prevention is key to avoiding Listeria infections. Dr. Gaither recommends avoiding the following foods during pregnancy:
- Deli meats and hot dogs unless reheated until steaming hot
- Refrigerated pate, meat spreads, or smoked seafood
- Unpasteurized milk and soft cheeses made from unpasteurized milk
- Raw or undercooked seafood, eggs, meat, or poultry
- Unwashed raw fruits and vegetables
- Ready-to-eat salads
- Unpasteurized juices
It is also important to seek medical care promptly if you or your newborn show any symptoms. If you live in an area affected by a food recall and have consumed any of the listed products, contact your healthcare provider immediately.