Accusations of Abuse and Neglect Surface at Kingstree Youth Facility
A Behavioral Treatment Facility Faces Allegations of Abuse and Neglect
A behavioral treatment facility in Williamsburg County, South Carolina, has come under scrutiny for multiple allegations involving sexual assault, physical abuse, and neglect. The facility, known as Broadstep Behavioral Health in Kingstree, is a 40-bed psychiatric residential treatment facility that serves children in foster care and those with special needs.
The facility treats individuals with intellectual and developmental disabilities and mental health conditions. It primarily houses children referred by agencies such as the Department of Social Services or parents who believe their children need more support.
A Parent's Experience
In 2020, Deeva Williams sent her son, Justin Williams, to Broadstep Kingstree based on a recommendation from their Department of Disabilities and Special Needs case worker. “As a parent, you don’t know everything that your child is dealing with and enduring back there. They go through that door in the back and you have no idea,” she said.
Justin, who was only 13 years old when he first entered the facility, has autism and suffers from serious depression, often experiencing suicidal thoughts. “I was more than just depressed; I couldn’t be alone at all because it was like every day it was a crisis,” he said.
Once inside the facility, Justin claimed his depression and suicidal thoughts were not only ignored but encouraged. “When I talk about things that were bothering me and that were done to me, it’s never handled, it’s never addressed,” he said. “The only excuse they would give you is, ‘Oh, I’m an adult, I can say what I want.’ They felt like they were judge, jury and executioner.”
Tragedy and Legal Consequences
One of Justin’s friends at the facility was physically and emotionally assaulted, leading to severe emotional distress. The teenager took his own life inside the facility on January 25, 2024. Court documents state that Broadstep did not properly file an investigative report following the death, which violated a state regulation.
“I was extremely angry. After that, yeah, I cried a lot,” Justin said. “It shouldn’t take somebody having to die before people realize the effect that they have on other people.”
Repeated Complaints and Violations
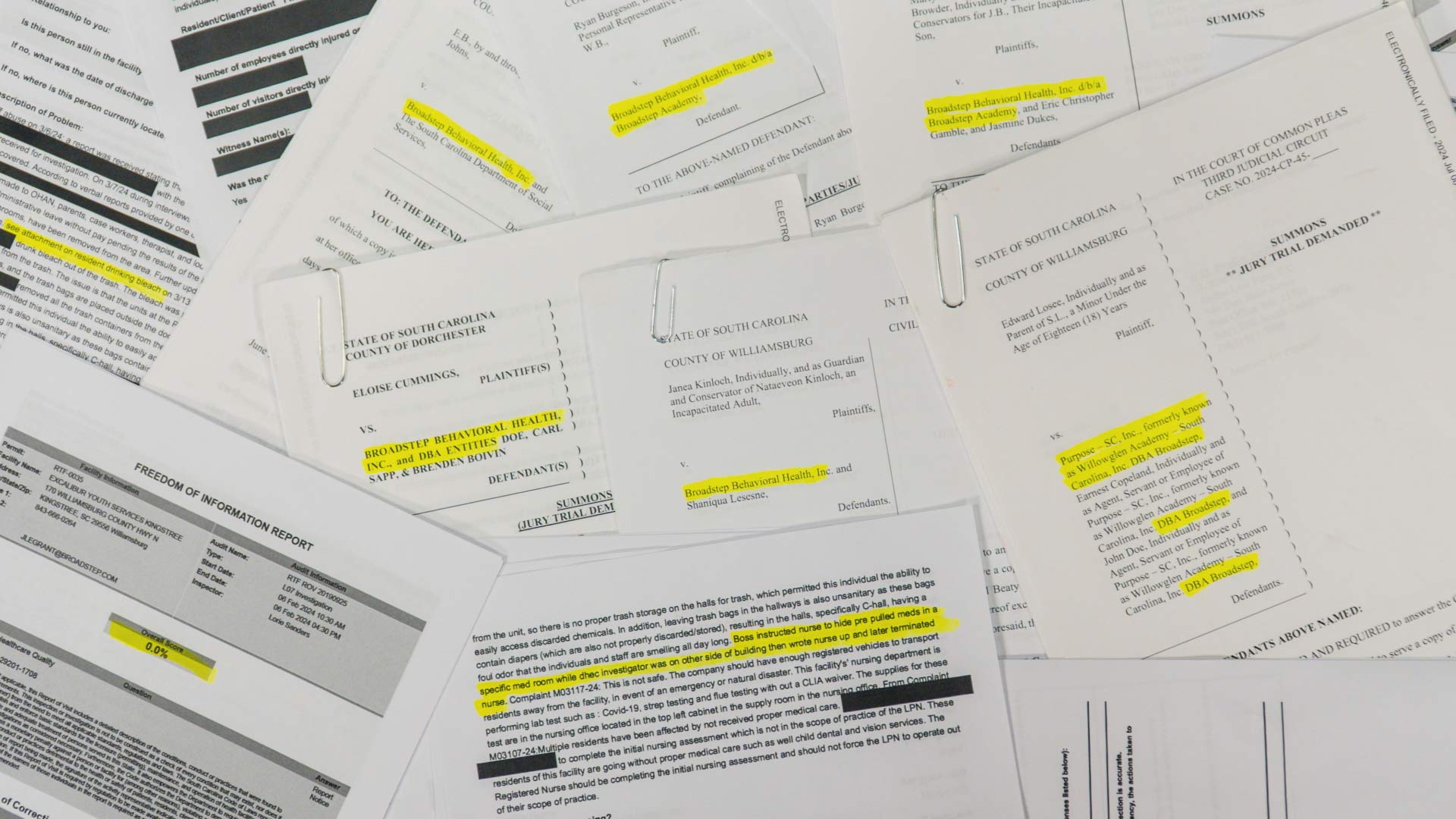
The situation at Broadstep Kingstree is far from isolated. The South Carolina Department of Public Health provided data showing dozens of complaints against the facility from 2023 until this year. These complaints include staff hitting, sitting on, and stepping on children, allowing children to fight, isolating them due to understaffing, improper medical care, bed bugs, residents escaping, emotional abuse, and sexual assault.

“Why is it that more vulnerable children can go to a daycare, go to somewhere where they’re supposed to be taken care of, and get this type of treatment?” Deeva Williams asked. “You are having to try and deal with this and put the pieces back together. We were already out of our depth.”
One complaint claims a patient was physically assaulted by a staff member and placed in restraints. Another states that a staff member slammed another patient into a wall. Another complaint alleges that a staff member poured bleach into a Welch’s grape juice bottle and threw it into the trash before a resident drank it, causing severe vomiting.
An additional complaint states a resident was found with shoe prints on their body, with a staff member claiming they accidentally stepped on the individual’s face.
Legal Representation and Ongoing Issues
“These facilities are shrouded in confidentiality and kind of secrecy protections under the law,” said Attorney Heather Hite, who has represented multiple clients against Broadstep. “These children haven’t done anything wrong to deserve the way that they’ve been treated.”
Hite has represented a then 13-year-old special needs child who was placed into Broadstep’s care. According to court documents, the girl experienced employees refusing to give residents water and blankets when they were cold. She also witnessed other children being restrained and strip-searched.
The 13-year-old was later moved to Broadstep’s Kingstree location, which the lawsuit claims was even worse. The girl reported being sexually assaulted by a maintenance man who entered her room.
“She was further abused and neglected. It made her needs — they were already bad — go from bad to worse,” Hite said.
State Agencies and Facility Responses
How is a facility like Broadstep still operating despite its history of abuse and neglect? After each complaint is filed, the South Carolina Department of Public Health (SCDPH) is required to inspect a facility. However, even when Broadstep failed inspections, the facility would provide a corrective action plan and claim improvements were made.
Yet, SCDPH allowed Broadstep to continue operating despite ongoing complaints and violations. “I think the people who run these companies, run these facilities, they should be held responsible because you’re dealing with these precious packages,” said Deeva Williams.
SCDPH declined an interview request but released a statement explaining its role in licensing and regulating facilities. The department stated it conducts inspections and investigations to ensure compliance with regulations. Since June 2024, SCDPH has conducted one routine inspection, two food and sanitation inspections, and five complaint investigations of Excalibur Youth Services Kingstree, resulting in eight cited violations.
DSS and DDSN did not respond to requests for comment. Broadstep’s corporate offices did not respond to three different requests for comment.
Continued Concerns
Despite the allegations, Broadstep continues to operate in several locations, including Simpsonville and Williamsburg. The company previously had locations in Georgetown, Pickens, and Simpsonville, but after media coverage, the Georgetown and Pickens locations closed down.
Broadstep also has a location open in Summerville that has faced lawsuits in recent years. However, SCDPH states that the facility is technically a group home, not a behavioral treatment facility, meaning the state agency does not oversee it.